What are Social Determinants of Health?
Social determinants of health (SDOH) are non-medical factors that influence a person's health outcomes. They are conditions in which people are born, grow, live, work, and age, and the wider set of forces and systems shaping the conditions of daily life. SDOHs have a major impact on people’s health, well-being, and quality of life, and present challenges for patients and their ability to receive care. They include factors like socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care. There are a growing number of initiatives to address social determinants of health within and outside of the health care system. The Office of the National Coordinator (ONC) hosts webinars and a Social Determinants of Health Information Exchange Learning Forum to provide resources and education on health equity and SDOH topics. For more information about how social determinants impact the health of a patient and other implementation resources, visit the following:
Importance of Taking Action
To most effectively provide care for patients, it is vital to gain a comprehensive understanding of what non-medical factors may be contributing or affecting the patient’s condition. A growing number of health sector and non-health sector and initiatives are emerging to address social determinants of health. Some non-health sector efforts include accessibility to public transportation, better early childhood education for low-income students, healthier corner stores in low-income communities, and other interventions. Health care delivery system efforts include multi-payor federal and state initiatives, as well as provider-level activities focused on identifying and addressing the non-medical social needs of patients through screenings and referrals to programs that can address the identified need. A patient's cultural may also play a role in care delivery and should be considered (see our Cultural Awareness web page). Follow these steps to implement a SDOH program in your practice:
Step 1: Select a screening tool relevant to the practice's patient population
Screening for SDOH helps to identify non-medical factors affecting a patient's health. The goal is to help the patient with their specific needs thus selecting the pertinent tools for your patient population, and for which the practice can provide resources or referrals, is important for success. It may be necessary to customize a screening tool by selecting elements from several of the various tools already available. Ultimately, the tool should be short, simple, and meaningful to the patient. The Kaiser Permanente screening tool finder filters tools based on the identified determinants and returns screening tools that address each condition selected. The following are some examples of peer-reviewed screening tools:
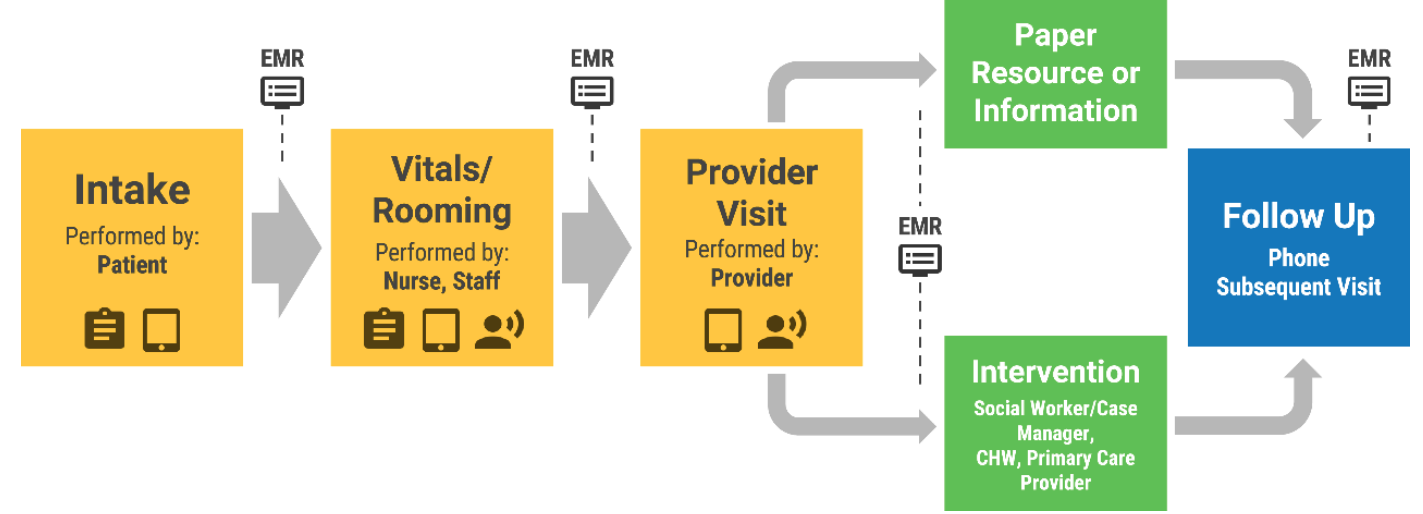
Step 2: Develop a workflow
- Decide who in the practice will perform the screening and how it will be executed (review the Everyone Project Team-Based Approach - Implementation Guide for assistance).
- Create screening tool selection criteria to determine which tool will be used for a given patient (see the Kaiser Permanente screening tool finder).
- Create a referral form/template to refer patients to needed resources, or use the AHRQ form.
- Determine how to prioritize the patient's needs.
- Establish a follow-up process to ensure patients receive the resources they need.
Step 3: Develop a list of referral resources and establish relationships
For your SDOH screening and referral efforts to be impactful, develop a list of referral resources/programs to connect patients to needed services in their community. Consider contacting and establishing relationships with those resources you utilize often for better collaboration. While not comprehensive, the below list of community resources can assist in identifying resources.
Step 4: Connect patients with resources
Establish processes that best fit your practice's capabilities to successfully connect patients with the needed community resources and programs. Develop an in-house program and designate a staff member to be a patient navigator, or partner with community resource groups that can act as a patient navigator. Consider utilizing digital solutions like apps, email, texts, and other automated outreach solutions.
- Patient Navigators - someone who supports patients and families through treatment and care, connects them to community resources, provides education on health conditions, helps to follow-up with providers, and guides patients across the care continuum
- Community Resource Coordination Groups (CRCGs) - County-based groups of local partners and community members that work with parents, caregivers, youth and adults to identify and coordinate services and supports, including behavioral health, basic needs and caregiver support. They help people whose needs can't be met by one single agency and who would benefit from interagency coordination.
- Insurance plan case management/care coordination - Navigate to the Payors section on the HCMS Billing and Payors page for links to health plan case management/care coordination.
- NowPow App - a personalized community referral platform that uses a digital platform and data analytics to connect patients in under-resourced neighborhoods to nearby vital health and social services.
Step 5: Identify reimbursement, coding, and documentation requirements:
Develop documentation, ICD.10, and CPT coding protocols to accurately report SDOH services provided. Collect this data to assess and refine your SDOH services. Correct coding may also assist payors in identifying patients with SDOH needs for possible intervention and outreach.
Additionally, when appropriate, bill for the SDOH screening using the applicable CPT and ICD.10 codes (see the
American Academy of Pediatrics for guidance). Also, screening for SDOH is now reflected in the evaluation and management (E/M)
Medical Decision Making (MDM) Table of Risk. Depending on the significance of the impact of a patient’s socioeconomic status on the diagnostic or treatment options, the encounter may be considered moderate risk reported with codes 99204 and 99214.
To capture data on the social needs of patients, applicable ICD-10-CM codes should be reported on the claim to identify non-medical factors that may influence a patient’s health status. A list of the SDOH diagnosis codes can be found in the ICD-10 manual in the
range of Z55-Z65 (code to the highest specificity). Check for coding updates regularly to avoid claim rejections/denials as the codes to report SDOH change frequently.
Additional Resources