Advanced endoscopy means skipping surgery
By Sarah Ravani STAFF WRITER
 Robin Jerstad / For the San Antonio Express-News
Robin Jerstad / For the San Antonio Express-News
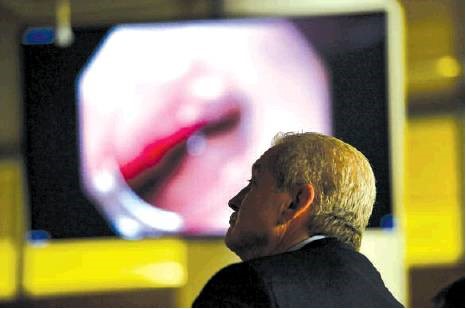
A University Health System gastroenterology and endoscopy team member watches livestreaming of advanced endoscopy procedures during a recent conference in San Antonio.
Roberto Baltierra was no stranger to anesthesia, a hospital gown or a hospital bed, though the insertion of an IV into his arm still made him feel queasy. Since March, he had been to different doctors about five times to remove a gallstone lodged in a bile duct.
But with each try came the discouraging news that doctors had been unsuccessful. Until Baltierra, 27, of San Antonio, received a call from Dr. Sandeep Patel, a gastroenterologist and medical director of the Advanced Endoscopy Program at University Health System.
“Dr. Patel looked into my case and saw what I’d been through,” Baltierra said. “He said, ‘Let me be your doctor and do this procedure on you.’ ”
Patel told Baltierra that he would use a laser “like a tiny jackhammer” to remove the stone, Baltierra added.
The procedure is known as an advanced endoscopy. A regular endoscopy is a nonsurgical procedure, using a tube with a light and camera inserted through the mouth or rectum, to examine the digestive tract and diagnose gastrointestinal disorders. With advanced endoscopies, physicians can also provide treatment through them.
“Advanced endoscopy is a field that’s growing. It’s an interventional field where the idea is to provide relief of acute and chronic diseases,” said Dr. Obi C. Ukabam, an advanced endoscopy fellow at University Hospital. “Procedures that were routinely done with open surgery can now be done with advanced endoscopy.”
One example of an advanced endoscopy is the endoscopic retrograde cholangio-pancreatography, which is when the endoscope is passed down the small bowel and into the bile duct and removes a stone that is stuck there. It can also detect cancers. There are also other advanced procedures, which include an endoscopic ultrasound and the laser lithotripsy.
“In an endoscopic ultrasound, it’s a scope that looks like a routine operative endoscope, but it has something at the end that probes,” Ukabam said.
The laser lithotripsy is the “tiny jackhammer” that Baltierra’s doctor used.
Endoscopic ultrasounds give physicians an opportunity to obtain a closer look at a patient’s chest cavity, pancreas, spleen, abdomen and gall bladder, Ukabam said.
“We can get a better view of the inside organs, better views than sometimes an MRI or CT scan because we are so close to the organs, from the inside looking out,” Ukabam said.
Baltierra’s procedure was one of about a dozen that was broadcast live last week to doctors and others attending the Texas Society for Gastroenterology and Endoscopy meeting in San Antonio. Some of the patients were at Baylor College of Medicine in Houston while others, such as Baltierra, were at University Hospital.
Plans for an advanced endoscopy center are underway at University Hospital as part of its expansion that includes the recently approved Women and Children’s Tower, said Donald Finley, a spokesman for University Health System.
The center will have bigger rooms to accommodate the growing workload, Finley said.
Currently, there are two advanced endoscopy rooms and four standard endoscopy rooms. The new center will have four advanced endoscopy rooms and six standard rooms.
The $390 million project is a major addition, which would increase the number of patients served and consolidate services for women and children.
University Hospital isn’t the only institution to offer advanced endoscopies in San Antonio. The South Texas Advanced Gastroenterology Center at Methodist Hospital also performs the procedures, as does San Antonio Gastroenterology Associates and Endoscopy Centers.
Some endoscopy centers, including GAB Endoscopy Center Ltd., do not offer advanced endoscopies.
Last week, doctors and nurses sat in a dark conference room at University Hospital, their eyes glued to the television screen as doctors just a floor above and in Houston performed advanced endoscopies while narrating their every move for the broadcast.
“We have different therapies, different techniques used, and so we are teaching our colleagues all over Texas how we do it and how to do it safely in the patient’s interests,” Ukabam said.
For Baltierra, several doctors had been unable to remove the stone for months. He had a plastic stent put in, which failed. Same with a metal stent several weeks later.
“I work in plumbing. I know what happens to pipes when something gets stuck in there. Water has to come out from somewhere,” Baltierra said. “It freaks me out. I’ve got a life to live. I don’t want to die.”
Before being wheeled into the examination room where his procedure would be broadcast, Baltierra felt like he had nothing to lose.
Even if part of the stone is removed, it’s better than nothing, he said.
By Wednesday, five days later, Baltierra was back to work. Patel had successfully removed the stone that had been plaguing Baltierra for nearly six months.
“I have to go for a checkup in six weeks, but it’s all good now,” Baltierra said in a text message. “Don’t feel any different, but it’s all good. From this point on, it’s on me now to stay healthy.” sravani@express-news.net
Leni Kirkman
Senior Vice President
Strategic Communications & Patient Relations
University Health System
4502 Medical Drive, MS 94-01
San Antonio, TX 78229